Affiliate Disclosure: This article contains affiliate links. If you purchase through these links, we may earn a commission at no additional cost to you. We only recommend products and programs that align with evidence-based approaches to gut health for weight loss.
The relationship between gut health for weight loss goes deeper than most people realize. Your digestive system houses trillions of microorganisms that directly influence whether your weight loss efforts succeed or fail. These microscopic residents control metabolism, hormone production, and even how many calories your body extracts from food.
Recent research reveals something remarkable: two people eating identical meals can experience completely different weight outcomes based solely on their gut bacteria composition. This isn’t speculation—controlled studies transferring gut microbiomes between individuals consistently demonstrate these effects. Your intestinal ecosystem matters as much as what you eat.
Most weight loss advice ignores this fundamental piece of the puzzle. Traditional calorie-counting misses how gut bacteria affect inflammation levels, hunger signals, and fat storage patterns. Understanding gut health for weight loss changes the entire approach to sustainable body composition management.
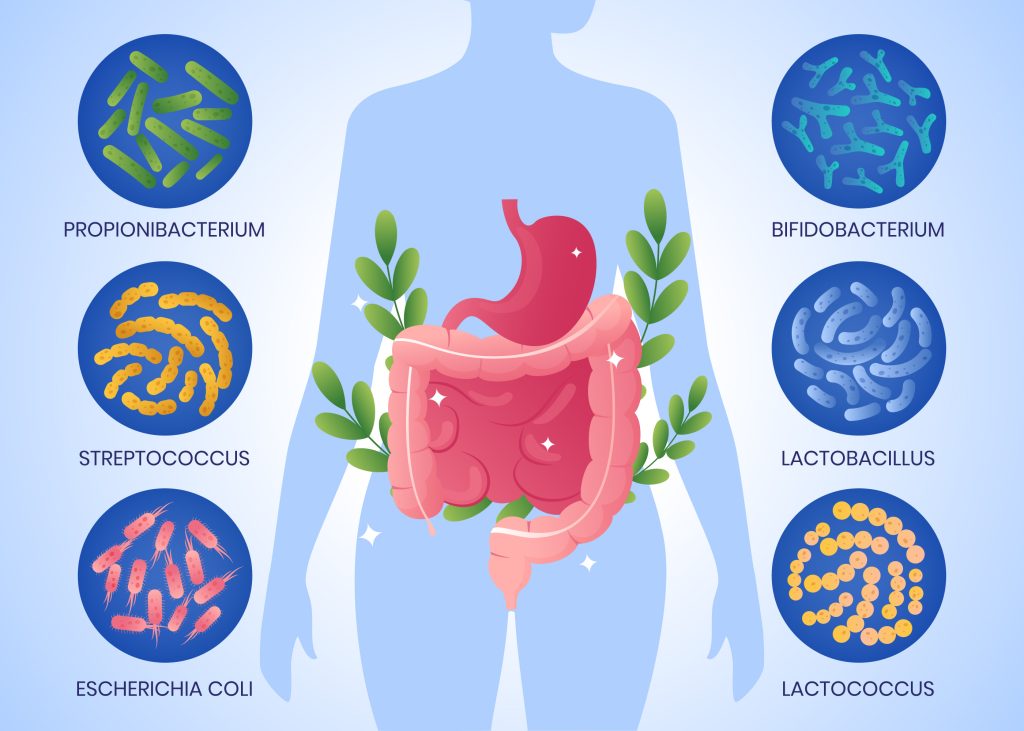
Scientists now identify specific bacterial strains that either support or sabotage weight management goals. Some microbes help you feel satisfied after reasonable portions. Others trigger constant hunger regardless of caloric intake. The difference between these populations determines long-term success more than willpower alone.
This guide examines the documented connections between intestinal bacteria and body weight regulation. You’ll discover which beneficial microbes support healthy weight loss, how dietary patterns cultivate them, and why optimizing your gut microbiome might resolve weight challenges that traditional approaches haven’t addressed.
Understanding Your Intestinal Microbiome
Your digestive tract contains approximately 100 trillion microorganisms spanning thousands of species. This complex community includes bacteria, fungi, viruses, and other microscopic life forms collectively called your gut microbiome. Each person’s composition differs as distinctly as a fingerprint, shaped by genetics, environment, diet, and lifestyle patterns.
The gut microbiome weighs roughly 2-3 pounds total. Despite this relatively small mass, these organisms perform critical functions affecting your entire body. They synthesize vitamins, break down complex carbohydrates, produce neurotransmitters, and communicate directly with immune cells.
Scientists classify gut bacteria into groups called phyla. The two dominant phyla in most people are Firmicutes and Bacteroidetes. Research suggests the ratio between these bacterial families correlates with body weight and metabolic health markers. Individuals with obesity tend to show higher Firmicutes to Bacteroidetes ratios compared to lean individuals, though this relationship proves more nuanced than initially thought.
Your microbiome develops from birth and continues evolving throughout life. Early childhood represents a critical window for establishing diverse bacterial communities. Birth method, breastfeeding patterns, antibiotic exposure, and environmental factors all shape this ecosystem during formative years.
Modern lifestyles significantly impact microbiome diversity. Processed foods, artificial sweeteners, chronic stress, inadequate sleep, and excessive antibiotic use all reduce bacterial variety. This diversity loss associates with numerous health problems, including difficulty maintaining healthy body composition.
The gut-brain axis represents another crucial aspect of microbiome function. Intestinal bacteria produce neurotransmitters like serotonin and GABA that influence mood, appetite, and food cravings. This bidirectional communication system explains why digestive health affects mental wellbeing and vice versa.
Your intestinal lining serves as a selective barrier, allowing beneficial nutrients to pass while blocking harmful substances. When bacterial populations become imbalanced—a condition called dysbiosis—this barrier can become compromised. Increased intestinal permeability may contribute to systemic inflammation and metabolic dysfunction that complicate weight management.
Different bacterial strains perform specialized roles. Some excel at fermenting dietary fiber into short-chain fatty acids that fuel intestinal cells. Others produce enzymes breaking down complex plant compounds. This functional diversity explains why microbiome composition matters more than simply bacterial quantity.
The Science Connecting Gut Bacteria to Body Weight
Research consistently demonstrates that people with obesity harbor distinctly different gut bacterial communities compared to individuals maintaining healthy weights. These differences aren’t coincidental—they directly influence how bodies process food, store fat, and regulate metabolism.
A landmark 2013 study published in Science examined gut bacteria transferred from human twins into mice. When researchers transplanted microbiomes from obese twins into germ-free mice, those mice gained significantly more weight and body fat than mice receiving bacteria from lean twins. This experiment proved gut bacteria can directly cause changes in body composition independent of diet or genetics.
The mechanisms linking gut health for weight loss involve multiple biological pathways. Certain bacterial strains increase energy extraction from food, meaning your body absorbs more calories from identical meals. Other microbes influence genes regulating fat storage and insulin sensitivity. Some produce metabolites reducing inflammation, while others generate compounds triggering inflammatory responses.
Short-chain fatty acids (SCFAs) represent one critical link between gut bacteria and metabolism. Beneficial microbes ferment dietary fiber into SCFAs like butyrate, propionate, and acetate. These compounds serve multiple functions: fueling intestinal cells, reducing inflammation, improving insulin sensitivity, and signaling satiety to your brain.
According to research from Washington University School of Medicine, individuals with lower gut bacterial diversity show increased insulin resistance and inflammation markers. These metabolic disturbances make weight loss significantly more challenging. The study found participants with more diverse microbiomes responded better to dietary interventions, suggesting that gut health for weight loss optimization should precede or accompany traditional diet changes.

Gut bacteria also influence appetite-regulating hormones. Certain strains stimulate production of GLP-1 and PYY—hormones promoting feelings of fullness. Other bacteria affect ghrelin, the hunger hormone. This explains why microbiome composition impacts whether you feel satisfied or constantly hungry, even when consuming adequate calories.
The endotoxin theory offers another explanation for the gut-obesity connection. Some intestinal bacteria produce lipopolysaccharides (LPS) that trigger low-grade systemic inflammation when entering the bloodstream. This metabolic endotoxemia contributes to insulin resistance, fat accumulation, and difficulty losing weight.
Bile acid metabolism represents an additional pathway where gut bacteria influence weight regulation. Your liver produces bile acids for fat digestion, but gut microbes transform these compounds into secondary bile acids. These modified molecules act as signaling compounds affecting metabolism, insulin sensitivity, and fat storage throughout your body.
Research published in Cell Metabolism identified specific bacterial species associated with successful weight loss outcomes. People with higher levels of Akkermansia muciniphila and certain Prevotella species lost more weight on identical diet plans compared to those lacking these bacteria. This finding suggests gut microbiome composition predicts individual weight loss potential.
Eating timing also interacts with gut bacteria to influence metabolism. Studies show gut microbiome composition fluctuates throughout the day in sync with circadian rhythms. Disrupting these natural patterns through irregular eating schedules or nighttime eating may negatively impact metabolic health and weight management efforts.
Key Gut Bacteria Supporting Healthy Weight Management
Specific bacterial strains demonstrate remarkable abilities to support healthy weight maintenance. Understanding these beneficial microbes helps inform decisions about cultivating a weight-management-friendly gut environment.
Akkermansia muciniphila stands out as one of the most promising bacteria for metabolic health. This species strengthens intestinal barriers, reduces inflammation, and improves insulin sensitivity. Research shows people with obesity typically have lower levels of A. muciniphila compared to lean individuals. Studies indicate that increasing this bacterium through dietary changes can enhance weight loss outcomes significantly.
Christensenella minuta represents another strain strongly associated with lower body weight. Scientists identified this bacterium as highly heritable and consistently more abundant in lean individuals. Animal studies demonstrate that introducing C. minuta into germ-free mice prevented weight gain even on high-fat diets. This species appears to influence metabolism in ways that protect against obesity.
Bifidobacterium species play multiple beneficial roles in weight management. These bacteria produce acetate, a short-chain fatty acid helping regulate fat storage and energy expenditure. Bifidobacterium also strengthens gut barrier function, reducing metabolic endotoxemia. Higher Bifidobacterium levels correlate with better glucose control and lower body fat percentages.
Lactobacillus strains offer varied effects on weight, with some species showing particularly promising results. Lactobacillus gasseri demonstrated weight loss benefits in clinical trials, with participants losing significant abdominal fat over 12 weeks. L. plantarum and L. rhamnosus also show potential for supporting healthy body composition.
Faecalibacterium prausnitzii produces large amounts of butyrate, a short-chain fatty acid with powerful anti-inflammatory properties. This bacterium associates with metabolic health markers and lower obesity risk. People with inflammatory bowel conditions, which often accompany weight management difficulties, typically show reduced F. prausnitzii levels.
Roseburia species excel at producing butyrate from dietary fiber. These bacteria correlate with improved insulin sensitivity and reduced inflammation. Studies link higher Roseburia abundance with lower body weight and better metabolic health markers, making them important targets for gut health for weight loss strategies.
The Prevotella copri strain shows interesting connections to carbohydrate metabolism. Research indicates people with higher P. copri levels may respond more favorably to high-fiber, plant-based diets for weight loss. This bacterium efficiently breaks down complex carbohydrates into beneficial metabolites.
Bacteroides thetaiotaomicron demonstrates impressive abilities to digest diverse plant polysaccharides. This species helps extract nutrients from vegetables and whole grains while producing metabolites influencing energy balance. Its presence supports dietary diversity and metabolic flexibility.
Conversely, some bacterial groups associate with weight gain and metabolic problems. Clostridium difficile overgrowth relates to inflammation and metabolic disturbances. Certain Firmicutes members at excessive levels may extract too much energy from food, contributing to unwanted weight gain.
How Gut Bacteria Influence Weight Gain Mechanisms
Understanding how gut bacteria affects weight gain reveals why microbiome optimization matters for sustainable management. These microscopic organisms affect your body through multiple interconnected pathways that either promote or prevent fat accumulation.
Energy harvesting efficiency varies dramatically based on gut bacterial composition. Some microbes extract significantly more calories from identical food compared to others. This means two people eating the same meals can absorb different caloric amounts based solely on their gut bacteria. Individuals with obesity-associated microbiomes may harvest up to 150 additional calories daily from their diet.
Inflammation regulation represents another critical mechanism. Certain gut bacteria produce compounds triggering chronic low-grade inflammation, a condition called metabolic endotoxemia. This inflammation disrupts insulin signaling, promotes fat storage, and makes weight loss extremely difficult. Anti-inflammatory bacterial strains help maintain metabolic health and support healthy body composition.
Appetite and satiety signals originate partially from your gut microbiome. Beneficial bacteria produce metabolites stimulating release of hormones like GLP-1 and PYY, which promote fullness after eating. Other microbes may interfere with these signals, leading to increased hunger and food cravings. This explains why optimizing gut health for weight loss significantly impacts dietary adherence.

Fat storage genes respond to signals from gut bacteria. Specific microbial metabolites can activate or suppress genes controlling how your body stores dietary fat. Some bacteria promote fat accumulation in adipose tissue, while others encourage fat burning and prevent excessive storage. This genetic regulation occurs without any changes to your DNA sequence.
Gut barrier integrity affects systemic metabolism. A healthy, diverse microbiome maintains tight junctions between intestinal cells, preventing unwanted substances from entering your bloodstream. When gut bacteria populations become imbalanced, intestinal permeability increases. This allows bacterial components and partially digested food particles to trigger immune responses and metabolic dysfunction.
Bile acid metabolism transforms how your body processes dietary fats. Primary bile acids from your liver get modified by gut bacteria into secondary bile acids. These transformed molecules act as signaling compounds influencing metabolism throughout your body. They affect insulin sensitivity, energy expenditure, and fat distribution patterns.
Vitamin and nutrient production by gut bacteria influences metabolic health. Certain strains synthesize B vitamins, vitamin K, and other compounds essential for energy metabolism. Deficiencies in these microbe-produced nutrients can impair metabolic function and contribute to weight gain over time.
Circadian rhythm disruption through microbiome imbalances affects weight regulation. Your gut bacteria population naturally fluctuates throughout the day. Irregular eating patterns, poor sleep, or shift work can disrupt these rhythms. Studies show that circadian misalignment in gut bacteria associates with increased obesity risk and metabolic syndrome.
Neurotransmitter production by intestinal bacteria affects eating behaviors. Your gut microbes produce or influence synthesis of serotonin, dopamine, and GABA—neurotransmitters regulating mood, stress response, and food-related decision making. Imbalances may contribute to emotional eating, food addiction, and difficulty maintaining healthy eating patterns.
Best Probiotics for Weight Loss and Gut Health
Probiotics offer a targeted approach to improving gut bacterial composition for weight management. These beneficial microorganisms can help shift your microbiome toward a healthier balance supporting your goals.
Lactobacillus gasseri shows the strongest evidence for weight loss benefits among probiotic strains. A 2013 Japanese study found that participants taking L. gasseri daily for 12 weeks lost an average of 8.5% abdominal visceral fat. This strain appears particularly effective at reducing belly fat, which poses the greatest health risks.
Lactobacillus rhamnosus demonstrates gender-specific effects on weight management. Research indicates this strain significantly benefits women’s weight loss efforts. A Canadian study found women taking L. rhamnosus lost twice as much weight during a diet period and continued losing weight during the maintenance phase, while men showed minimal effects.
Bifidobacterium lactis (also called B. animalis) improves multiple metabolic markers related to weight. Studies show this probiotic reduces body fat percentage, improves insulin sensitivity, and decreases inflammation markers. It works synergistically with dietary changes rather than producing effects in isolation.

Lactobacillus plantarum helps reduce body fat accumulation, particularly when combined with fiber-rich diets. This strain excels at breaking down plant compounds and producing beneficial metabolites. Research suggests L. plantarum may prevent fat storage by modulating genes involved in lipid metabolism.
Multi-strain formulations often outperform single-strain products for weight management. Studies using combinations of Lactobacillus and Bifidobacterium species show enhanced benefits compared to individual strains. The synergistic effects of multiple beneficial bacteria may better replicate a healthy, diverse microbiome.
Saccharomyces boulardii, a beneficial yeast rather than bacteria, supports gut health in complementary ways. While not directly promoting weight loss, this probiotic helps maintain intestinal barrier function and reduces inflammation. It proves particularly useful after antibiotic treatment, which can disrupt weight-regulating gut bacteria.
Akkermansia muciniphila represents an emerging probiotic showing tremendous promise for gut health for weight loss applications. Though not yet widely available in supplements, ongoing research explores how to harness this bacterium’s benefits. Some studies indicate that pasteurized A. muciniphila may actually work better than live versions for improving metabolism.
When selecting probiotics for weight management, colony-forming units (CFUs) matter significantly. Research suggests effective doses typically range from 10 billion to 100 billion CFUs daily. However, more doesn’t always mean better—strain specificity and viability matter more than sheer numbers.
Delivery method affects probiotic survival and effectiveness. Delayed-release capsules protect bacteria from stomach acid, ensuring they reach your intestines alive. Some formulations include prebiotics (fiber feeding beneficial bacteria), creating synbiotic supplements that may enhance colonization success.
Fermented foods provide natural probiotics with additional nutritional benefits. Yogurt containing live cultures, kefir, sauerkraut, kimchi, miso, and kombucha all deliver beneficial bacteria along with bioactive compounds. Regular consumption of diverse fermented foods may provide advantages over supplement-only approaches.
Timing and consistency influence probiotic effectiveness. Most research indicates taking probiotics daily produces better results than sporadic use. Taking them with meals may improve bacterial survival, though some strains work better on an empty stomach. Consistency matters more than perfect timing.
Quality control concerns plague the probiotic supplement industry. Third-party testing reveals many products contain fewer viable bacteria than labeled or include incorrect strains. Look for brands with transparent testing, specific strain identification, and appropriate storage recommendations.
Microbiome Diet Plan for Beginners
Creating a gut-friendly eating pattern doesn’t require extreme restrictions or complicated protocols. This practical microbiome diet plan focuses on nourishing beneficial bacteria while minimizing foods promoting dysbiosis.
Week 1-2: Foundation Building
Start by adding fermented foods to your daily routine. Begin with small portions—just 2-3 tablespoons of sauerkraut, kimchi, or kefir with one meal daily. This gradual introduction prevents digestive discomfort while allowing beneficial bacteria to establish themselves. Choose unpasteurized versions when possible, as heat treatment kills live cultures.
Increase fiber intake gradually to feed your good gut bacteria. Target an additional 5 grams of fiber daily this week from whole food sources. Focus on diversity: berries, leafy greens, beans, oats, and root vegetables. Each plant food contains unique prebiotic compounds nourishing different bacterial strains.
Eliminate artificial sweeteners completely. Research shows compounds like sucralose, aspartame, and saccharin alter gut bacteria composition in ways that may promote glucose intolerance and weight gain. Replace diet sodas with water infused with fruit or herbal tea.
Week 3-4: Diversification
Expand your fermented food variety to include at least three different types weekly. Try yogurt with live cultures at breakfast, miso soup with lunch, and kimchi with dinner. This diversity introduces various beneficial bacterial strains to your gut ecosystem.

Aim for 30 different plant foods weekly, as recommended by research from the American Gut Project. This includes all vegetables, fruits, whole grains, legumes, nuts, and seeds. Higher plant diversity correlates with increased microbiome diversity, which associates with better metabolic health and easier weight management.
Add prebiotic-rich foods strategically. Include Jerusalem artichokes, onions, garlic, leeks, asparagus, and underripe bananas. These foods contain inulin and other fibers specifically feeding beneficial bacteria. Start with cooked versions, which are easier to digest than raw preparations.
Week 5-6: Optimization for Gut Health for Weight Loss
Incorporate resistant starch foods that bypass digestion and feed gut bacteria. Cooked and cooled potatoes, rice, and pasta develop resistant starch during cooling. Green bananas, cashews, and oats also provide this beneficial compound. Target 15-20 grams of resistant starch daily.
Include polyphenol-rich foods supporting beneficial bacteria growth. Blueberries, dark chocolate (70%+ cacao), green tea, extra virgin olive oil, and colorful vegetables provide polyphenols. These plant compounds act as prebiotics and possess anti-inflammatory properties supporting metabolic health.
Reduce processed food consumption to less than 10% of total calories. Ultra-processed foods often contain emulsifiers, preservatives, and additives disrupting gut bacteria. Research links high processed food intake with reduced microbiome diversity and increased obesity risk.
Ongoing Maintenance
Establish regular meal timing to support your gut bacteria’s circadian rhythms. Eating at consistent times helps maintain healthy microbial fluctuations throughout the day. Avoid late-night eating, which disrupts these natural patterns and may promote weight gain.
Stay hydrated with at least 8 cups of water daily. Adequate hydration supports mucus production in your intestines, which feeds A. muciniphila and other beneficial bacteria. Dehydration can alter gut bacteria composition negatively.
Limit alcohol consumption, which directly harms beneficial gut bacteria while promoting harmful strains. If you drink, red wine in moderation provides polyphenols that may partially offset negative effects. However, even moderate alcohol consumption can disrupt microbiome balance.
Foods to Emphasize:
- Fermented vegetables (sauerkraut, kimchi, pickles)
- Fermented dairy (yogurt, kefir, aged cheese)
- Diverse vegetables (aim for rainbow colors)
- Whole grains (oats, quinoa, barley, brown rice)
- Legumes (lentils, chickpeas, black beans)
- Nuts and seeds (walnuts, almonds, chia, flax)
- Prebiotic vegetables (onions, garlic, asparagus)
- Polyphenol-rich foods (berries, tea, dark chocolate)
Foods to Minimize:
- Artificial sweeteners and sugar alcohols
- Emulsifiers (carrageenan, polysorbate-80)
- Ultra-processed foods with long ingredient lists
- Excessive red meat (limit to 2-3 servings weekly)
- Fried foods and trans fats
- Refined sugars and syrups
- Excessive alcohol
Lifestyle Factors That Influence Gut Health and Weight
Your daily habits profoundly impact gut bacterial composition beyond dietary choices alone. These lifestyle factors can either support or undermine your microbiome-based weight management efforts.
Sleep Quality and Duration
Insufficient sleep devastates gut microbiome health and weight regulation. Research shows just two nights of poor sleep can alter gut bacteria composition in ways promoting weight gain. Sleep deprivation decreases beneficial Bacteroidetes while increasing Firmicutes populations associated with obesity.
Aim for 7-9 hours of quality sleep nightly. Establish consistent sleep-wake times, even on weekends, to support both circadian rhythms and microbial balance. Your gut bacteria follow daily patterns that sync with sleep-wake cycles. Disrupting these rhythms through irregular sleep schedules can trigger metabolic dysfunction.
Create an optimal sleep environment: completely dark, cool (65-68°F), and free from electronic device blue light exposure. These conditions support melatonin production, which influences gut bacteria populations. Research indicates melatonin directly affects microbiome composition and metabolic health.
Stress Management
Chronic stress dramatically alters gut bacteria composition through the gut-brain axis. Stress hormones like cortisol directly impact intestinal permeability and bacterial populations. Studies show that chronic stress reduces beneficial bacteria while allowing potentially harmful strains to proliferate.
The connection works bidirectionally—poor gut health also increases stress sensitivity and anxiety. This creates a cycle where stress harms your microbiome, which then makes you more vulnerable to stress effects.
Implement daily stress-reduction practices: meditation, deep breathing exercises, yoga, or nature walks. Even 10-15 minutes of mindfulness practice daily can positively influence gut bacteria composition. Research demonstrates that meditation practitioners harbor more diverse microbiomes compared to non-meditators.
Physical Activity
Exercise independently shapes gut microbiome composition beyond its calorie-burning effects. Studies show athletes possess more diverse gut bacteria and higher levels of butyrate-producing species compared to sedentary individuals. These differences exist even when controlling for diet.
Moderate exercise appears optimal for microbiome health. Aim for 150 minutes of moderate-intensity activity weekly, as recommended by health authorities. Activities like brisk walking, cycling, swimming, or dancing all positively influence gut bacteria.
Excessive high-intensity training without adequate recovery may actually harm gut health. Studies on ultra-endurance athletes show signs of increased intestinal permeability and microbiome disturbances. Balance intense workouts with adequate rest and recovery periods.
Antibiotic Stewardship
Antibiotics represent one of the most destructive influences on gut microbiome diversity. A single course of broad-spectrum antibiotics can eliminate beneficial bacterial strains for months or even years. Some research suggests permanent microbiome changes following repeated antibiotic exposure.
Take antibiotics only when medically necessary for bacterial infections. They’re ineffective against viral illnesses like colds and flu. When antibiotics are required, discuss narrow-spectrum options with your healthcare provider to minimize collateral damage to beneficial bacteria.
Support microbiome recovery after antibiotic treatment. Increase fermented food consumption, take high-quality probiotics (starting after completing the antibiotic course), and maximize dietary diversity. Research shows aggressive microbiome support following antibiotics can accelerate recovery.
Environmental Exposures
Contact with natural environments and diverse microbes supports gut health. Studies demonstrate that people who spend more time outdoors, garden regularly, or own pets harbor more diverse microbiomes. This “rewilding” of gut bacteria may protect against obesity and metabolic diseases.
Reduce exposure to antimicrobial chemicals in household products. Triclosan, found in some soaps and cleaning products, can disrupt gut bacteria composition. Choose simple soap and water for hand washing instead of antibacterial products for routine use.
Social Connection
Social interactions influence gut microbiome composition through shared microbial exposures. People living together develop increasingly similar gut bacteria over time. Research even shows that social isolation in animals alters microbiome composition in ways affecting brain chemistry and behavior.
Maintain regular social connections with friends and family. Share meals together, which promotes both emotional wellbeing and microbial exchange. These social factors contribute to the overall ecosystem of influences on your gut health and weight management success.
Tracking Your Progress with Gut Health for Weight Loss
Monitoring improvements helps maintain motivation and refine your approach for optimal results. Several methods exist for assessing microbiome changes and their effects on weight management.
Subjective Health Markers
Pay attention to digestive symptoms as initial indicators of gut health changes. Track bowel movement frequency, consistency, and regularity using the Bristol Stool Chart as reference. Healthy gut function typically produces Type 3 or 4 stools (smooth, soft, and easy to pass) daily or every other day.
Monitor energy levels throughout the day, particularly afternoon energy crashes or post-meal fatigue. Improved gut health often corresponds with more stable energy and reduced afternoon slumps. Keep a simple daily log rating energy from 1-10 at wake-up, midday, and evening.
Notice changes in food cravings, particularly for sugar and ultra-processed foods. As beneficial gut bacteria increase, many people report reduced cravings for unhealthy foods. This shift reflects changes in gut-brain signaling rather than pure willpower.
Track mood and mental clarity as gut-brain axis indicators. Many people experience improved mood, reduced anxiety, and better focus as gut health improves. Consider using a simple mood tracking app or journal entry to identify patterns over weeks and months.
Body Composition Changes
Weight measurements provide one data point, but body composition offers more valuable information. Track measurements weekly at the same time of day (morning after bathroom, before eating). Include waist circumference, hip circumference, and waist-to-hip ratio alongside scale weight.
Progress photos every 2-4 weeks reveal changes that scales and measurements might miss. Take consistent photos in the same lighting, location, and poses. Body composition shifts often become visible before significant scale changes occur.
Consider body fat percentage testing if available. Methods range from simple bioelectrical impedance scales to more accurate DEXA scans. While individual measurements may vary, trends over months provide useful feedback about your interventions.
Functional Health Markers
Monitor fasting blood glucose using an inexpensive home glucometer. Improved gut health often corresponds with better glucose regulation. Target fasting glucose of 70-99 mg/dL. Check weekly at the same time each morning for consistent comparisons.
Blood pressure tracking provides insight into cardiovascular health improvements that often accompany better gut health and weight loss. Check blood pressure at rest, ideally same time daily. Look for gradual trends toward normal ranges (below 120/80 mmHg).
Microbiome Testing
Direct microbiome analysis through stool testing offers the most detailed assessment. Commercial tests analyzing gut bacteria composition provide reports on bacterial diversity, beneficial species abundance, and personalized dietary recommendations.
These tests typically cost $99-299 and require mailing a small stool sample to a laboratory. Results show which bacterial species inhabit your gut, diversity scores, and comparisons to healthy populations. Some services offer periodic retesting to track microbiome changes over time.
Consider baseline testing before starting significant dietary or lifestyle changes, then retest after 3-6 months of consistent intervention. This timeline allows sufficient microbiome shifts to become measurable while maintaining reasonable testing costs.
Creating Your Tracking System
Develop a simple, sustainable tracking routine that doesn’t become burdensome. Weekly check-ins work better than daily measurements for most markers. Use a smartphone app, spreadsheet, or journal—whichever system you’ll actually maintain consistently.
Focus on trends over individual data points. Week-to-week fluctuations are normal and don’t indicate failure. Look for patterns over 4-8 weeks to assess whether your interventions are working.
Celebrate non-scale victories alongside weight changes. Improved digestion, better energy, reduced cravings, and enhanced mood all indicate successful optimization, even before significant weight loss occurs.
Common Mistakes and How to Avoid Them
Many people sabotage their optimization efforts through well-intentioned but misguided approaches. Recognizing these common pitfalls helps you maintain progress toward your goals.
Taking Too Many Supplements
The supplement industry markets countless products promising benefits, leading many people to consume excessive pills and powders simultaneously. This scattershot approach wastes money and may actually harm your microbiome through unexpected interactions or overwhelming bacterial populations.
Focus on 1-2 high-quality, research-backed supplements at most. Prioritize food-based approaches first, using supplements only to address specific gaps. Give each supplement adequate time (4-6 weeks minimum) to assess effectiveness before adding another product.
Neglecting Food Quality
Some people focus exclusively on adding probiotics while continuing to eat a diet dominated by processed foods. Beneficial bacteria can’t thrive in an environment of artificial additives, emulsifiers, and excessive sugar. It’s like planting seeds in contaminated soil—they simply won’t grow.
Remember that dietary changes provide the foundation for improvements. Probiotics and supplements work best when combined with a whole-foods-based eating pattern rich in fiber and diverse plant foods. You can’t supplement your way out of a poor diet.
Expecting Immediate Results
Microbiome changes occur gradually over weeks and months, not days. Many people give up on gut-healthy approaches after just one or two weeks without visible weight loss. This short-sighted approach prevents you from experiencing the genuine benefits that develop with consistent effort.
Commit to at least 12 weeks of consistent gut-friendly eating and lifestyle practices before evaluating results. Significant microbiome shifts typically require 4-8 weeks, with body composition changes following several weeks later. Patience is essential for sustainable success.
Ignoring Individual Variation
Generic “one-size-fits-all” approaches often fail because everyone’s microbiome is unique. A probiotic strain that works brilliantly for your friend might provide no benefits for you. Dietary changes improving one person’s gut bacteria could have minimal effect on someone else’s microbiome.
Pay attention to your body’s specific responses rather than blindly following popular protocols. Keep detailed notes about which interventions correlate with improvements in your energy, digestion, mood, and weight. This personalized approach outperforms rigid adherence to generic plans.
Overdoing Fermented Foods
Enthusiasm for fermented foods sometimes leads people to consume excessive amounts, particularly when starting out. This can trigger digestive distress including bloating, gas, and diarrhea. Your gut needs time to adapt to increased probiotic bacteria populations.
Start with small portions (1-2 tablespoons) and gradually increase over several weeks as your system adapts. Listen to your body’s feedback about portion sizes and frequency. Some people thrive on large amounts of fermented foods, while others function best with more moderate consumption.
Neglecting Prebiotic Fiber
Many people focus exclusively on probiotics (beneficial bacteria themselves) while ignoring prebiotics (the fiber feeding those bacteria). Without adequate prebiotic fuel, probiotic bacteria struggle to establish themselves and thrive in your gut.
Ensure your diet includes ample prebiotic-rich foods: onions, garlic, leeks, asparagus, Jerusalem artichokes, oats, and underripe bananas. Aim for at least 25-35 grams of total fiber daily from diverse plant sources. This combination of probiotics and prebiotics creates optimal conditions for microbiome improvement.
Inconsistent Implementation
Sporadic efforts with gut-friendly foods and practices produce minimal results. Your gut bacteria respond to consistent environmental signals over time. Yo-yoing between healthy and unhealthy patterns prevents stable microbiome improvements.
Develop sustainable habits you can maintain long-term rather than extreme short-term interventions. Small, consistent actions compound into significant microbiome changes over months. Focus on progress, not perfection, while maintaining general consistency with your approach.
Conclusion
Your gut health for weight loss represents a powerful, science-backed approach to achieving and maintaining healthy body composition. The trillions of microorganisms in your digestive system influence metabolism, appetite regulation, inflammation, and fat storage in ways that profoundly impact your success.
Research continues revealing sophisticated connections between gut bacteria and body weight. Specific beneficial strains like Akkermansia muciniphila, Christensenella minuta, and various Lactobacillus species support healthy outcomes through multiple mechanisms. Meanwhile, microbiome imbalances and reduced bacterial diversity associate with obesity and metabolic dysfunction.
The practical strategies outlined in this guide—emphasizing fermented foods, diverse plant fibers, strategic probiotics, and supportive lifestyle habits—provide actionable steps for optimizing your gut microbiome. These approaches work synergistically with traditional methods while addressing root causes that standard calorie-counting often misses.
Remember that microbiome optimization requires patience and consistency. Significant changes develop over weeks and months, not days. Your unique bacterial composition means that personalized attention to your body’s specific responses outperforms rigid adherence to generic protocols.
The connection between gut health and weight loss extends beyond simple pounds on a scale. Improved energy, better mood, reduced cravings, and enhanced overall wellbeing accompany successful microbiome optimization. These benefits make the journey worthwhile regardless of specific numbers.
Start with small, sustainable changes rather than overwhelming yourself with complete dietary overhauls. Add one fermented food daily, increase plant diversity gradually, prioritize sleep and stress management, and give your gut bacteria time to respond. These incremental improvements compound into significant results over time.
Your gut microbiome represents a modifiable factor in weight management that you can influence through daily choices. By understanding and nurturing your gut health for weight loss, you unlock your body’s natural capacity for reaching and maintaining a healthy weight sustainably.
P.S. Ready to take the next step in optimizing your gut health for weight loss? offers comprehensive support with evidence-based formulations designed to promote beneficial gut bacteria and support your weight management journey. Start your transformation today.

